Skin Health: Prevention and Treatment of Skin Breakdown
Originally Published in The Siegel Rare Neuroimmune Association Journal
Volume V
January 2011
Janet Dean, MS, RN, CRRN, CRNP
The International Center for Spinal Cord Injury
Kennedy Krieger Institute, Baltimore Maryland
Skin is the largest organ covering the entire outside of the body. It receives one third of the body’s blood circulation. Your skin is tough and pliable, forming the body’s protective shield against heat, light, chemical and physical action. It plays an active role with the immune system, protecting us from infection. Your skin maintains a stable internal environment and is important in maintaining a proper temperature for the body to function well. In addition to providing protection and internal regulation, your skin gathers sensory information from the environment, allowing you to feel painful and pleasant stimulation. Your skin also stores water, fat, and vitamin D.
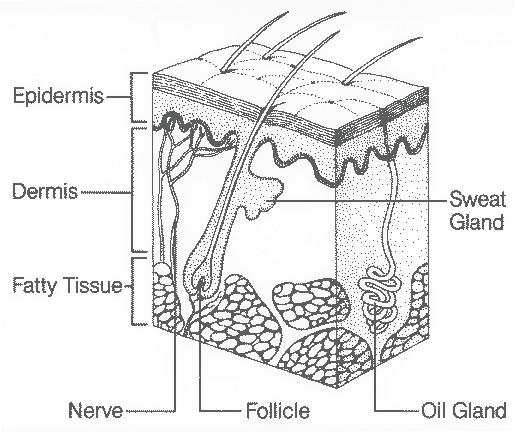
The skin consists of three layers: Epidermis, dermis, and subcutaneous tissue. The outermost layer, the epidermis, is composed mostly of dead skin cells that are constantly being shed and replaced. The dermis or second layer has sweat glands, oil glands, nerve endings, and small blood vessels called capillaries, which are all woven together by a protein called collagen. Collagen provides nourishment and support for skin cells. The nerves ending in this layer transmit sensations of pain, itch, touch and pleasure. The hair follicles also originate in this layer. Destruction of either the epidermis or dermis can leave the body open and susceptible to infection. The subcutaneous adipose tissue is the deepest layer of skin and is a layer of fat and collagen that houses larger blood vessels and nerves. This layer is important in controlling the temperature of the skin itself and the body and protects the body from injury by acting as a shock absorber. The thickness of this layer varies throughout the body and from person to person. Underneath the subcutaneous tissue lays muscle and bone.
For the most part, the skin is tough, pliable and resistant to injury. If the skin becomes injured or broken, it is generally very resilient and has an amazing ability to self-repair and heal. Despite this resiliency, the skin is susceptible to breakdown, if subjected to prolonged abuses, such as excessive pressure, shear force, friction or moisture. This is a major concern for persons with transverse myelitis or other neuroimmunologic conditions that cause paralysis and/or decreased sensation.
For people with paralysis, the skin is at increased risk for breakdown for several reasons. Paralysis itself affects the skin and underlying tissue. There is loss of collagen which weakens the skin and makes it less elastic. The lack of muscle function around boney areas of the body leads to muscle atrophy, resulting in less padding, which in turn, adds to the risk of skin breakdown. People with paralysis often have difficulty shifting their weight, repositioning themselves, or transferring without assistance.
Impaired sensation is often present, limiting the ability to sense when to make a weight shift or position adjustment. People with impaired sensation are also vulnerable to injury from many other hazards, such as, heat, cold, sun and trauma. Loss of sensation put an individual at risk for burns from very ordinary activities, such as using a lap top computer sitting directly on your lap or sitting too close to a fireplace. Injury can be caused from things that are too cold such as, ice packs or cold exposure causing frostbite. Ingrown toenails can become infected and sunburn can become severe without feeling it.
When limited mobility is coupled with decreased sensation, a person is more likely to develop a specific type of skin breakdown called a pressure ulcer. According to the National Pressure Ulcer Advisory Panel, a pressure ulcer is defined as a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction (1). Pressure ulcers are one of the leading causes of complication across the life span of persons with paralysis (2). Up to 95 % of adults with spinal cord injury will develop at least one serious pressure ulcer at some time during their life (3).
Skin breakdown can range from minor scrapes, cuts, tears, blisters or burns to the most serious pressure ulcers with the destruction of tissue down to and even including the bone. A pressure ulcer, especially one that requires surgery, such as a muscle flap or skin graft, can cost thousands of dollars to treat, require lengthy hospitalization, and weeks to months away from family, work, school or community activities. It has been estimated that for persons with spinal cord injury the cost of care for pressure ulcers is about $1.2 to 1.3 billion dollars annually (4).
With a concerted effort, skin breakdown is, for the most part, preventable. It can occur, however, even in people who maintain the most diligent care and use the proper equipment. If skin breakdown is identified early, when still in the minor stages, and if the cause of the breakdown can be identified and eliminated, healing should occur fairly quickly. If it is not identified in its early stages, skin breakdown can rapidly progress from minor to serious.
Skin breakdown is caused in several different ways, including friction, shear, moisture and pressure. These causes can occur individually or in combination. Friction, moisture and sheer are identified as contributing factors to pressure ulcers (5). A friction injury occurs when the skin rubs on surfaces, such as a bed sheet, arm rest or brace and has the appearance of a scrape, abrasion or blister. This type of injury is typically seen on the heels and elbows and may result from repositioning, propping or rubbing due to increased spasticity.
A shearing injury occurs with dragging or sliding of a body part across a surface and has the appearance of a cut or tear. This type of injury can occur from dragging your bottom during a transfer or sliding down in bed when the head of the bed is elevated. With the sliding force, bone is moved against the subcutaneous tissue while the epidermis and dermis remains essentially in the same position; against the supporting surface such as a wheelchair or bed. This action causes occlusion of the blood vessels, decreasing blood flow, oxygen and nourishment to the skin, which eventually leads to breakdown. Sometimes a shear injury will actually tear the tissue over the tailbone and with unrelieved pressure will become a pressure ulcer.
Too much moisture over-hydrates the skin, making it weak and more sensitive to friction, shear and breakdown (think about being in the tub or pool for a long time). Primary sources of excess skin moisture include sweating, bowel and bladder accidents, and drainage from wounds.
Pressure ulcers occur when skin, soft tissue and blood vessels are compressed or squeezed between a bony prominence (such as your tailbone) and an external surface (such as your wheelchair cushion). With compression of these vessels, the blood that nourishes the cells and takes away waste is cut off, starving the tissue of oxygen and vital nutrients. Without food and oxygen, tissue dies and skin breakdown begins. The body tries to compensate by sending more blood to the area. This process results in redness and swelling, places even more pressure on the blood vessels, and further endangers the health of the skin and underlying tissue. Ultimately, a pressure ulcer forms. Increased pressure over short periods of time and slight pressure over long periods of time have been shown to cause equal amounts of damage.
Many factors have been identified as responsible for the development of skin breakdown and pressure ulcer formation. In addition to immobility, impaired sensation and the external factors described above, many internal contributing factors have been identified. These internal factors include poor nutrition and hydration, weight, impaired circulation and oxygenation, impaired cognition or thinking, substance abuse, depression and age (6, 7). Nutritional factors important to prevent or heal wounds include a balanced diet with an adequate intake of protein, vitamin C, vitamin A, and zinc, as well as an adequate intake of fluids (8). When a person is overweight, extra pounds place extra pressure on vulnerable skin areas increasing the risk of compression of blood vessels. Individuals that are underweight often have decreased muscle mass with less fat padding over boney areas leaving them vulnerable to skin breakdown. Smoking, diabetes, anemia and other vascular conditions all lead to decreased circulation, increasing risk for skin breakdown. Individuals who are depressed or have impaired thinking and judgment due to substance abuse are less likely to be vigilant with regard to important self-care issues, such as skin health. Young children generally have more resilient and elastic skin and more baby fat and padding so they often have very little difficulty with skin break down. As children move into adolescence, their skin loses some of its elasticity. They generally have more body weight, putting more stress on pressure areas, such as the ischeal tuberosicties and tailbone with sitting. Teens often begin to have more difficulty with skin breakdown. As we continue to age, our skin becomes increasingly less pliable and resilient. We experience the loss of collagen and muscle mass, as well as decreased circulation, making the skin more vulnerable. The elderly are most prone to skin tears and stripping due to fragile, thin, and vulnerable skin. In addition, incontinence may become a more frequent issue for bedridden or ill persons, increasing problems with moisture as described above.
How can I keep my skin healthy?
Take responsibility for you own skin care
The first line of defense in keeping your skin healthy is to take responsibility for your own skin care. If you are at risk for skin breakdown, you will need to develop a daily routine for monitoring and caring for your skin. You should do a complete inspection of your skin every day. If you are unable to assess your own skin, you should be knowledgeable about the areas of your body where you are most vulnerable to skin breakdown and be sure that your care givers are checking these areas for you and reporting the status of your skin.
The most common areas for skin breakdown (pressure points) in adults are the sacrum/coccyx (tailbone), heels, elbows, lateral maleollus (outside of the ankle), greater trocater (hip bone) or the bottom of the femur (outside and inside of the knee) and the ischial tuberosities (the bones we sit on). Pressure points for children are different and based on age and development (7). For infants and children less than three years of age, the head makes up a greater portion of the total body weight and surface areas. When they are placed on their backs, the occipital region (back of the head) becomes the primary pressure point. When placed on their side, the ears are also very susceptible. For older children, the sacrum (lower spine) and calcaneous (the heel of the foot) are most at risk (9).
Teach children to take responsibility for their own skin care
Parents of children at risk for skin breakdown need to be sure to check their children’s skin every day. This can become more difficult as children enter their teen years, develop more modesty and are interested (or insistent) on being more independent in their own care. This may be an area that parents need to insist on participation as skin breakdown can progress from minor to serious literally overnight in a child (or in an adult for that matter). If you have made daily skin inspection a part of your child’s routine since the onset of paralysis, this should be less of an issue. Be sure that they have the equipment, such as a mirror on a flexible wand, to inspect their own skin with your oversight, if at all possible.
Prevent mechanical Injury
Prevent mechanical injury to the skin from friction and shearing forces during repositioning and transfers. Lift, don’t slide. Lowering the head of the bed will help minimize sheer and friction from sliding down in bed. Raise the entire bed up to the proper height to facilitate level surface transfers to and from a wheelchair. If necessary, use assistive devices, such as transfer boards or mechanical lifts to help with transfers. Your physical or occupational therapist can help you with training and obtaining the correct equipment. Ensure that clothing fits comfortably and does not have pressure points, such as snaps, thick seams or pockets. Be sure that clothing is smoothed down under the bottom and back so you don’t get pressure points from bunched fabric. Keep bed sheets as wrinkle free as possible.
Keep skin clean and dry
Bathe frequently using mild soap. Avoid very hot water as it dries skin. Dry your skin by patting rather than rubbing. Change undergarments or pads as soon as possible after a bowel or bladder accident.
Eat a healthy diet
Eat a healthy diet and drink lots of fluids, especially water. Keep your body weight in a healthy range. People that are overweight or underweight tend to have more problems with skin breakdown. Good nutrition will help make your skin more resistant to breakdown and you will be more likely to heal and fight off infection should it occur. Eat the right kinds of foods. This means a balanced diet with servings from all food groups. For healthy skin it is especially important to get enough of the following nutrients in your diet:
- Omega 3 fatty acids (salmon, mackerel, flaxseed)
- Vitamin C (citrus fruits, strawberries, broccoli)
- Vitamin A (Vegetables that are dark green or dark orange in color)
- Zinc (seafood, meat and eggs)
- Protein (meat, eggs, cheese, and soy products)
Extra calories, especially from protein, are important for repairing damaged tissues if you do have skin breakdown. If you are concerned that you do not get enough of these foods in your diet, you can speak with a nutritionist or your health care provider about supplementation.
Develop a good home rehabilitation program
A regular daily therapy program will contribute to your overall health and well being, as well as reduce the risk of skin breakdown. A good program should include therapy to increase muscle mass and strength, improve your flexibility, improve your cardiovascular endurance, and increase your circulation. An activity based program that includes components of weight bearing and/or gait training, functional electrical stimulation biking, as well as strengthening and stretching activities are beneficial to help prevent skin breakdown. Use of the Wii gaming system in creative ways for “Wiihab” can help with improving strength, balance and endurance. Aquatic therapy and horseback riding therapy are also beneficial, in addition to being fun.
Avoid prolonged pressure on any one spot
Reposition frequently. When seated in a wheelchair, do weight shifts every 15 minutes. When lying in bed, reposition every 2 – 4 hours. Use pillows or wedges behind your back and between bony areas, such as knees and ankles. “Float” your heels and ankles off of the bed by supporting your lower leg with a pillow. Keep the head of the bed up less than 30 degrees to prevent shearing of skin from sliding down or the need to be pulled back up. If you use a wheelchair most of the day, avoid lying on your back at night. Instead, turn side to side to give your backside a break. Better yet, sleep on your stomach, if this position is comfortable and you are able to breathe safely. When positioned on your stomach, you have fewer pressure points, and can generally turn less frequently. Being on your stomach gives your backside a break, and allows you to stretch your hip flexor muscles and hamstring muscles, all for the price of one!
Use therapeutic surfaces
Therapeutic surfaces, such as a pressure relieving wheelchair cushion or a pressure relieving mattress will reduce or relieve pressure, promote blood flow to tissues and enable proper positioning. Make sure that you use equipment the way it is recommended and that it fits correctly. When seated in a wheelchair, make sure the cushion is properly positioned and inflated and that you are sitting all the way back in the wheelchair.
Keep muscle spasms under control
Some muscle spasms can be beneficial as they help you change position, if you can’t move yourself. Too much muscle spasticity can cause rubbing and friction, especially when you are in bed at night. Talk with your care provider about how to best manage spasticity. Exercise and range of motion are two good ways to reduce spasticity. Make sure orthotics (braces) are fitting properly, that they are worn correctly, and that the straps are fastened properly to prevent friction or pressure. Be sure that your bladder and bowel programs are working well as increased spasticity can be caused by a urinary tract infection or constipation. Spasticity can also increase when you have a burn or skin breakdown.
Identifying and treating minor skin breakdown
What does minor skin breakdown look like?
Skin breakdown starts out as a red or purple spot on fair skin or a shiny, purple, blue or darker spot on dark skin, which does not fade or go away within 20 minutes. When you press on the spot with your finger, it does not become lighter (blanch). It may feel warmer or cooler than the skin around it. The spot may feel hard or squishy under your fingers and may look swollen. If you have sensation, it may be itchy or painful. At first, it may not look like much, especially if the skin is not broken or open, but it can get a lot worse. If your skin becomes blistered, scabbed or has a small open area on the surface, this is more serious, as it indicates that the tissue underneath has begun to die. At this stage, the progression of skin break down is reversible: the skin will return to normal as soon as the cause of the irritation is found and eliminated and the skin is properly cared for. If these steps are not taken, the damage can rapidly progress to a dangerous level where infection can attack the underlying tissue and bone, posing a serious risk to your health.
Treating redness or minor skin breakdown
If the skin is open, contact your health care provider for wound care instructions. These instructions will generally include cleaning the area with soap and water or a saline solution, keeping the area dry, and eliminating the cause of the problem. Do not use hydrogen peroxide or iodine as these products damage new skin cells in the wound. They may prescribe special dressing that will optimize healing. If not, cover the area with a non-stick dressing, such as a Telfa pad to protect it from clothing. Change the dressing one to two times per day or if it gets soiled. Check your skin frequently to be sure the area is not getting worse. Minor burns can also cause blistering and can be treated in the same manner. If the burn covers a large surface area, you should seek care in the emergency room. Once a treatment plan has been established, you must identify and try to remove the source of the irritation to the affected area as much as possible.
Is the damage being caused by pressure during sitting?
Pressure areas caused by sitting often occur on your ischeal tuberocities (sitting bones), lower back, shoulder blades or the back of the heels. If the skin sore is being caused by sitting, check your wheelchair cushion. Do you have a pressure relieving cushion prescribed by your health care provider? Is it inflated correctly? Some cushions require frequent monitoring of inflation and can leak. Could the cushion be placed backward in the chair? Is it in good repair? Some cushions have gel in them that can get hard or squished out of place. If you have a therapeutic cushion and are still having difficulty with pressure on your sitting bones, see if you can try different cushions with pressure mapping. Pressure mapping equipment allows clinicians to visually identify your specific pressure areas when sitting on different cushions. Then the cushion that works best for you can be ordered. Pressure mapping can also be helpful, if you have a condition that can make seating difficult. Conditions, such as scoliosis or a dislocated hip can make the pressure on you sitting bones unequal. Depending on how bad the skin breakdown is you may need to stay out of your wheelchair for a period of time to allow the area to heal.
Is the damage being caused by pressure from lying on the area?
The areas most vulnerable when lying are the back of the head (in young children), ankles, knees, hips or shoulder blades. If so, avoid positioning on the affected area. If you have difficulty with red areas despite frequent turning, there are various pressure relieving mattresses that can be prescribed by your health care provider to distribute pressure better than a regular mattress. Unfortunately, if you have never had any skin breakdown, it is difficult to get insurance coverage for this type of specialty mattress. If you have had skin breakdown, coverage is often available.
Does the area of damage look more like a scrape or a tear?
If the area looks more like a scrape or tear, it may be caused by friction or sheer from sliding down in bed or wheelchair or from dragging your bottom with transfers. If you have had a change in your physical status, consider returning to physical therapy for a “tune up” focusing on increasing your strength, flexibility, and transfer technique. If you are dependent on others for part or all of your transfers, there is equipment that can be helpful to prevent sheer injury. This includes transfer boards, starting with simple slippery wood boards to a b-easy board with a sliding disk, a mechanical lifting device or overhead track lift systems. Your physical therapist and occupational therapist can help you identify equipment that will be most helpful for you and teach you and your care givers how to safely use this equipment. A hospital bed that raises and lowers and has an elevating head and foot rest can be helpful, especially if you require assistance from others for bathing, positioning and transfers. The ability to raise and lower the bed will protect your caregiver’s back and often allows for level or “downhill” transfers, avoiding sheer injuries. Manual (hand crank) hospital beds or semi-electric hospital beds (hand crank to raise and lower the bed and electric to elevate the head and foot) are often covered by insurance with a good letter of medical necessity from your health care provider. Ask your health care provider to order a fully electric hospital bed, if you are unable to operate a hand crank independently. Your health care provider should indicate that you require assistance with transfers and bed mobility and require frequent repositioning to prevent costly skin breakdown. If you prefer not to have a hospital bed, you can permanently raise the height of your entire bed so that it is even with your wheelchair using blocks of wood, bricks or bed leg adjusters that can be purchased.
Is the area of damage under a brace?
If redness persists greater than 20 minutes after removing the brace, do not wear the brace. Have your therapist or orthotist evaluate the brace to see if it can be adjusted or whether it will need to be remade. Children may need adjustments or replacement of braces as often as every four to six months during growth spurts. Braces will often require adjustment, if you have lost or gained weight, have increased spasticity, decreased range of motion or worsening scoliosis.
Is the redness or breakdown in the diaper (perineal) area?
Skin breakdown in the perineal area is generally caused by too much moisture often from sweating or irritation from urine and stool. Skin problems in this area start out as redness and swelling (rash) and can progress to vesicles or pimples with oozing, crusting or scaling. Once the skin is open, there is increased risk for infection. Perineal skin care should be done as soon as possible after a bowel and/or bladder accident. Gently wash the area with soap that is indicated for the perineal area. Regular bar soap or antibacterial soap used for routine skin care can dry out this skin. The skin in this area will need moisturization with products such as glycerin, lanolin or mineral oil to replace natural moisture that is lost with frequent cleaning. A skin barrier ointment or creams should be used to protect the skin from moisture or irritation.
If the redness or rash last longer than three days, has areas of multiple red bumps or pimples, or if you have oozing pimples that develop into a honey-colored crusted area, you should be seen by a heath professional as you may need treatment for a yeast infection or an antibiotic. Under-pads or absorbent briefs can be used as long as they wick moisture away, rather than trapping the moisture against the skin. Lastly, try to identify the cause of the skin irritation, especially if from frequent bowel or bladder accidents.
Identifying and treating serious skin breakdown
What does serious skin breakdown look like?
Serious skin breakdown occurs when the cause of the problem is not eliminated and tissue has been deprived of oxygen and nutrients for so long that the tissue has died and there is now a large hole or crater. Damage extends at least into the subcutaneous tissue. In the most serious wounds, tissue death includes muscle and extends as deep as the bone. Drainage is almost always present. If you have fever, see green or yellow drainage, and have a warm temperature around the wound, you may have developed an infection. Wounds such as this, with or without infection, must be evaluated by a health care professional. This care may be obtained through your spinal cord injury provider or you may be referred to a wound center to be evaluated and treated by a professional that specializes in the treatment of serious wounds. When an infection forms in a wound, the surrounding tissue and bone can become infected. If this continues, infection can enter the blood stream causing sepsis; and if untreated, can be fatal.
How is serious skin breakdown treated?
If the wound is not infected, you may be able to be treated at home with bed rest and frequent dressing changes. You should be evaluated by a wound care professional to identify the appropriate treatment plan and dressings. Specialized dressings are important to provide a moist environment for healing. Moist wounds heal faster than dry wounds. It is easier for a wound in a moist environment to granulate or grow new cells and for the cells to move across the wound bed. A moist environment increases the effectiveness of white blood cells in fighting infection, removing waste and dead tissue. Specialized dressings are also important to be sure that the wound heals from the inside out. If the wound heals from the outside first, it can trap infection inside that will later flare up and cause the wound to reopen. Deeper wounds need specialized wound care, including the removal of dead tissue either by special wound dressing or ointments (chemical debridement) or surgical removal of this tissue. This will then be followed by special dressings and packing material that can absorb drainage, remove dead tissue and then help the body heal itself. If a wound is draining heavily, a special dressing should be used to contain the drainage.
The most serious wounds, those that extend to the bone or have signs of infection, will require hospitalization for treatment. This will mean several weeks of bed rest with aggressive wound management and IV antibiotics. Aggressive treatment in a hospital that has a specialized wound care team can help you avoid surgery. Newer wound treatment and dressings can speed healing. Many hospital and wound centers use vacuum assisted closure therapy, hyperbaric oxygen therapy and electrical stimulation either directly in the wound or in the tissue surrounding the wound. Electrical stimulation should not be used if there is any chance that the underlying bone may be infected (osteomyelitis). If non-surgical treatment fails, or the wound is very severe, surgery will be required. Most often this will involve a muscle flap and skin grafting to close the wound and prevent reoccurrence of skin breakdown. This type of surgery generally costs thousands of dollars and requires a period of weeks in the hospital followed by several more weeks at home or in the hospital on a specialized bed. The total process is often 6 – 8 or 10 weeks before you can begin a gradual reseating program.
Conclusion
While it is well know that preventing skin breakdown is much easier than treatment and that there are many identified risk factors that can be modified to prevent skin breakdown, we know this is only part of the issue. In the real world, even with the best self-care or the best caregivers, you can develop skin breakdown if unexpected events or changes in your life occur. Remember, the threat of skin breakdown never subsides and, in fact, increases with aging and with the length of time from your diagnosis or injury. It is easy to become over confident or even lax in maintaining prevention habits the longer you have gone without having skin breakdown. Be increasingly vigilant with unexpected changes in your circumstance. Changes, such the loss of a trusted care giver or increasing responsibilities at home, work or school, can increase the risk to your skin. Sudden breakage of equipment also places you at increased risk. Being proactive and assertive in monitoring, maintaining and replacing broken or worn out equipment, such as wheelchair cushions is very important. Lastly, if you have a problem with skin breakdown, take charge immediately. Seek out professional help before it becomes serious.
Reference list
- National Pressure Ulcer Advisory Panel. Updated staging system of the national pressure ulcer advisory panel. February, 2007. https://www.npuap.org/pr2.htm. Last accessed December 3, 2010.
- Krause JS, Carter RE, Pickelsimer EE, Wilson D. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2008;89:1482-91.
- Jackson J, Carlson M, Rubayi S, Scott MD, Atkins MS, Blanche EI, Saunders-Newton C, Mielke S, Wolfe MK, Clark FA. Qualitative study of principles pertaining to lifestyle and pressure ulcer risk in adults with spinal cord injury. Disabil Rehabil. 2010;32(7):567-78.
- Regan MA, Teasell RW, Wolfe DL, Keast D, Mortenson WB, Aubut JA, Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil. 2009;90(2):213-31.
- Garber SL, Rintala DH. Pressure ulcers in veterans with spinal cord injury: a retrospective study. J Rehabil Res Dev. 2003;40(5):433-41.
- Jackson J, Carlson M, Rubayi S, Scott MD, Atkins MS, Blanche EI, Saunders-Newton C, Mielke S, Wolfe MK, Clark FA. Qualitative study of principles pertaining to lifestyle and pressure ulcer risk in adults with spinal cord injury. Disabil Rehabil. 2010;32(7):567-78.
- Butler CT. Pediatric skin care: Guidelines for assessment, prevention, and treatment. Ped Nurs. 2006;32(5):443-450.
- National Pressure Ulcer Advisory Panel. The role of nutrition in pressure ulcer prevention and treatment: National pressure ulcer advisory panel white paper. 2009. https://www.npuap.org/
- Baharestani MM, Ratliff CR. Pressure ulcers in neonates and children: An NPUAP white paper. Advan Skin & Wound Care. 2007;20(4):208-220.